PART 3.1
Implementing the smallpox surveillance and containment strategy required massive resources, commitment, and coordination. But moving from a traditional strategy, used for over a century and a half with clearly defined roles for every participant, to a new strategy simply seemed too labor intensive and impossible. This required mobilizing and coordinating hundreds of thousands of implementers with a gradual increase in the number of people involved.
PART 4.2
Women and their babies were dying from complications of home labor and delivery. Nana and her colleagues were pretty sure that they understood the problem. They thought this was happening because when the women went into labor they had no way to get themselves to their local healthcare facility. They thought that transportation to healthcare facilities that was local, affordable, and accessible was needed. Yet even after MAZA implemented motorized tricycles operated by local drivers in the community to transport women to healthcare facilities, the women were not going to the healthcare facilities.
PART 5.3
Infants were dying in rural health centers because they had complications that couldn't be dealt with in those hospitals. Doctors thought that a way to address this would be to transfer them to a larger hospital with more neonatal capacity. But, when the transfer solution was tried, it turned out that more infants were dying. Lives were not being saved. Babies continued to die because the transportation to the secondary or tertiary facilities took so long. The infants could not survive the trip.
PART 6.2
In Mozambique, there was local distrust of the health clinic. A woman did come into the health clinic to deliver her child but both she and the child died in childbirth. The doctor, Hans Rosling, felt terrible and worried that he would never regain the trust of the people in the surrounding villages. But he learned that it was important for him to return the bodies to the village for a proper burial as a sign of respect for the local culture.
PART 6.3
Gun violence research sought ways to prevent unnecessary gun deaths, disabilities, and anxiety. Many gun owners opposed research by the CDC on gun violence prevention because they believed that the goal of the research was to take their guns away. But the rise of mass school shootings led to a change in perspective because everyone was concerned about the safety of their children.
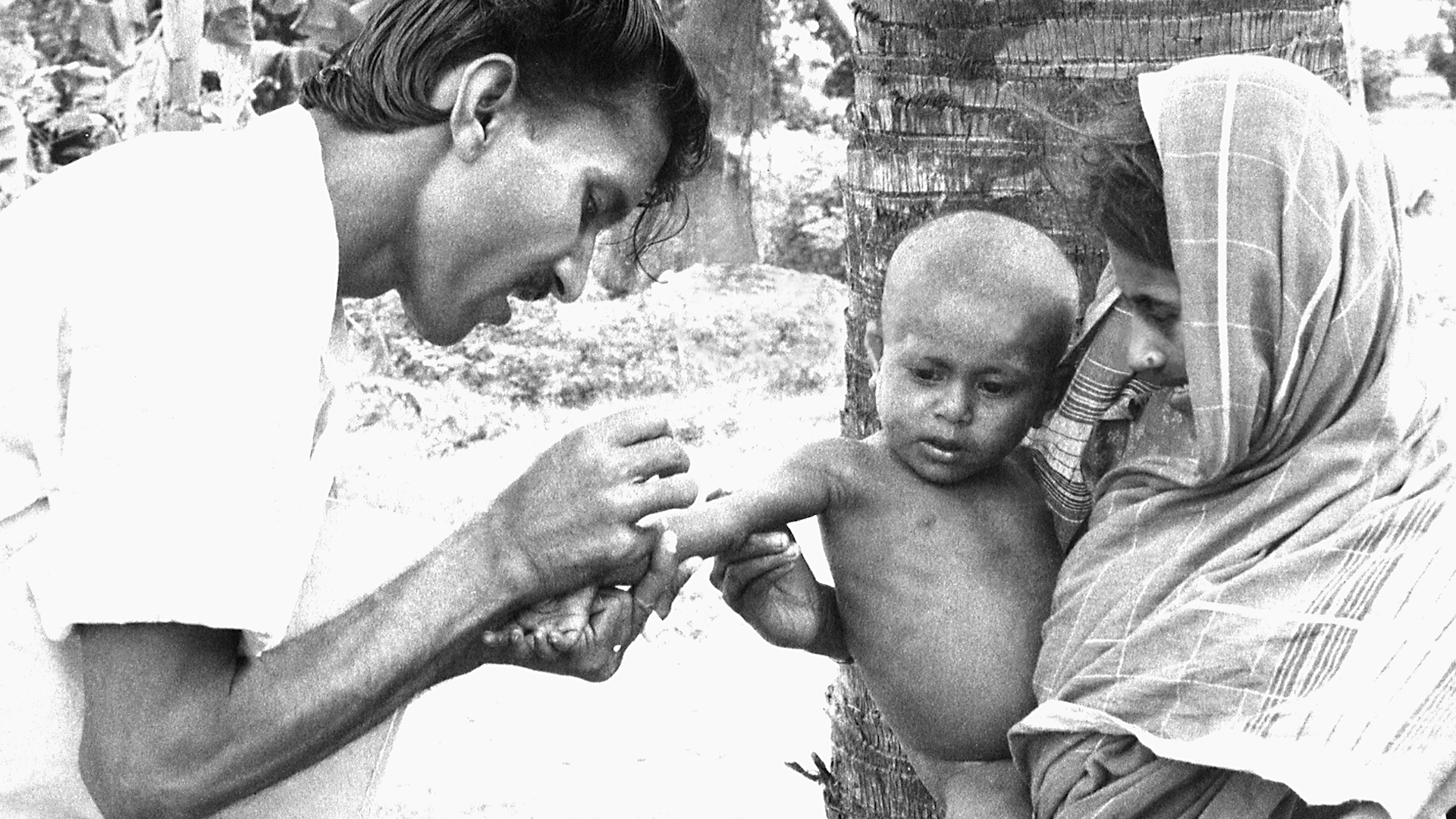
PART 7.1
In early 1974, smallpox outbreaks were appearing in areas of India that had been smallpox-free for months. After a week of plotting the epidemic with pushpins on hand-drawn maps, a pattern emerged. Each outbreak began with a working-age young man who had returned home to his village. These cases were “importations.” The young men had come from—or traveled through—the bordering state of Bihar. Cases were originating in Tatanagar, the company town of the corporate behemoth, Tata Companies. Tatanagar, a city in the state of Bihar, had no centralized government, and no public health structure in place.
PART 7.2
One of the most challenging things for vaccinations is reaching those who live “at the end of the road”—those who are geographically isolated due to distance or living in hard to access regions. A well-functioning delivery system is one that reaches the patient at the point-of-care. Such a system is essential for adequate access to and availability of vaccines. But, while across Africa, governments and donors are investing billions of dollars to strengthen health systems and make affordable medicines available, government supply chains often struggle to get medicines and supplies through the last mile to the health facilities and to the people who need them most.
PART 8.1
In 1973 India had thousands of cases of smallpox. For a while they were reporting one thousand new cases every day. Leaders of the eradication effort wanted to solicit help from WHO and bring in physicians, epidemiologists and health worker volunteers from other countries to supplement the Indian teams. But the Minister of Health for India felt that India had plenty of health workers and volunteers to do the job and said that people from other countries were not needed. The Minister's support for the smallpox effort was essential, so the team had to convince him to support bringing in workers from other countries without being critical of the great resources India already had.
PART 8.2
In Senegal, young girls usually had to go through a painful process deeply embedded in the culture of their society that served no purpose, and had been going on generation after generation. Girls and women were advocating for an end to this practice of female genital cutting. But their pleas were not enough to convince men throughout the country to stop this traditional cultural practice.
PART 8.3
In February 2016, the World Health Organization declared the Zika virus outbreak a Public Health Emergency of International Concern. The Latin America and Caribbean (LAC) region was the most affected with more than 700,000 cases reported. In response to the outbreak, the U.S. Government allocated a portion of the funds remaining from the previous Ebola outbreak response to the LAC region. But money was not enough. The region lacked the public health and laboratory infrastructure for disease surveillance, contact tracing, and diagnostics, and needed to quickly build a workforce to respond and prevent future outbreaks.
PART 9.3
There are medicines that could save the lives of the 500,000 children who die from malaria each year. Most of these children live in the low-income countries of Sub-Saharan Africa. Novartis manufactures the drug, artemisinin-based combination therapy, that is the standard of care for the treatment of P. falciparum malaria, the most deadly form of the disease. Although the global health community has for a long time been skeptical and wary of the private sector where profit was the driving force, Novartis happened to have a CEO who came from the field of global health and was inspired by the vision of global health equity. But neither these malaria-endemic countries nor WHO could afford to purchase commercially the amounts of this drug needed to treat the children who were at risk.