PART 5.1
In the battle to eradicate smallpox in India in 1974, finding and containing thousands of outbreaks was the key to getting smallpox under control. In mid 1974, the number of new outbreaks was starting to decrease slightly. The strategy of surveillance and containment - which included a massive workforce, tireless efforts, and rewards for identifying new cases - was paying off. But then we started to notice that members of previously vaccinated families were still coming down with smallpox. We should not have been seeing these new cases.
PART 7.1
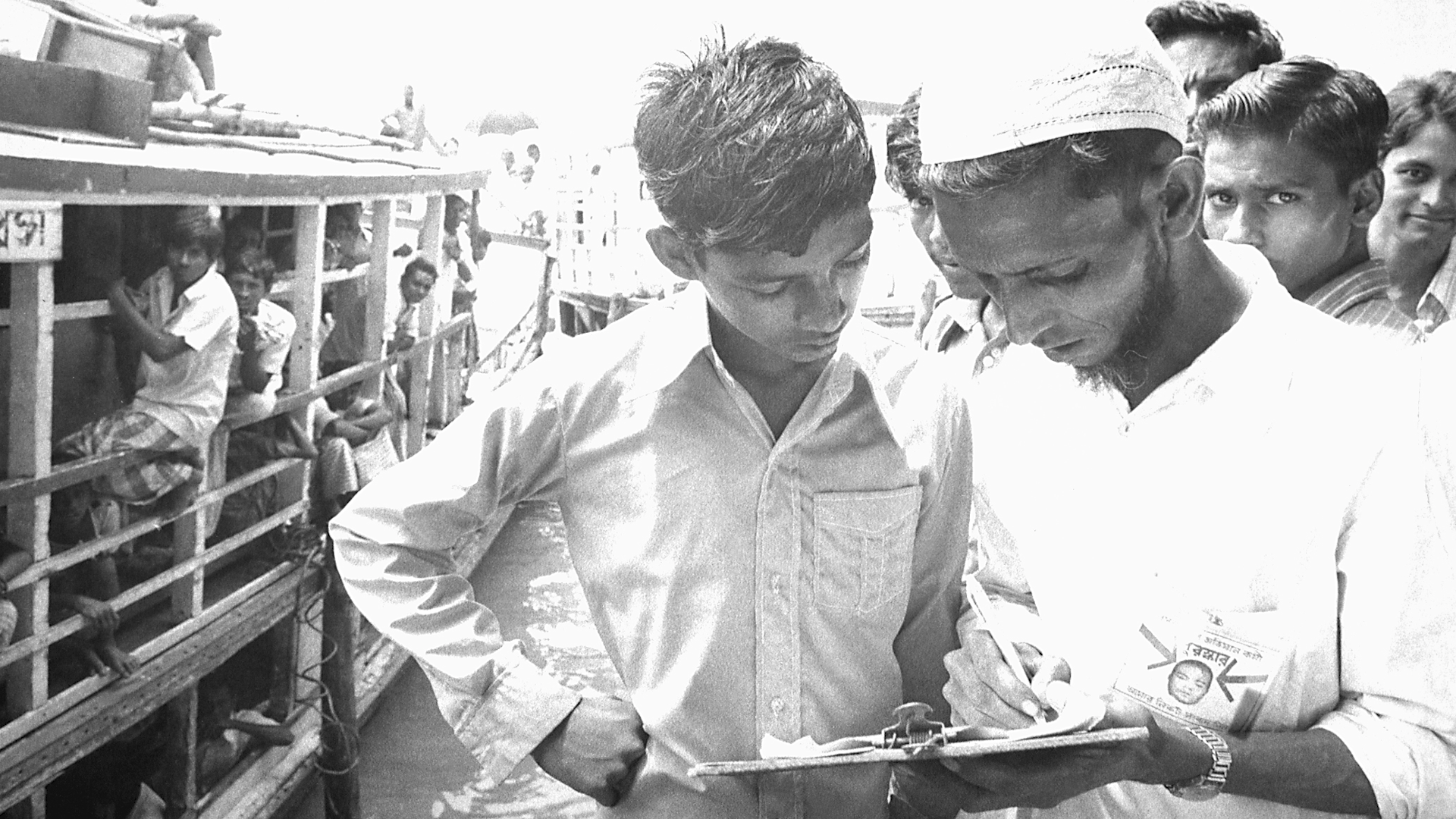
In early 1974, smallpox outbreaks were appearing in areas of India that had been smallpox-free for months. After a week of plotting the epidemic with pushpins on hand-drawn maps, a pattern emerged. Each outbreak began with a working-age young man who had returned home to his village. These cases were “importations.” The young men had come from—or traveled through—the bordering state of Bihar. Cases were originating in Tatanagar, the company town of the corporate behemoth, Tata Companies. Tatanagar, a city in the state of Bihar, had no centralized government, and no public health structure in place.
PART 8.2
In Senegal, young girls usually had to go through a painful process deeply embedded in the culture of their society that served no purpose, and had been going on generation after generation. Girls and women were advocating for an end to this practice of female genital cutting. But their pleas were not enough to convince men throughout the country to stop this traditional cultural practice.
PART 8.3
In February 2016, the World Health Organization declared the Zika virus outbreak a Public Health Emergency of International Concern. The Latin America and Caribbean (LAC) region was the most affected with more than 700,000 cases reported. In response to the outbreak, the U.S. Government allocated a portion of the funds remaining from the previous Ebola outbreak response to the LAC region. But money was not enough. The region lacked the public health and laboratory infrastructure for disease surveillance, contact tracing, and diagnostics, and needed to quickly build a workforce to respond and prevent future outbreaks.
PART 9.1
An effective vaccine for preventing smallpox had been discovered and tested by 1796. And by the 1970’s widespread vaccination resulted in most people in rich countries being vaccinated and almost completely protected. Smallpox was actually eliminated from developed countries in the 1970s. But the burden of smallpox was inequitably distributed. People in some poor countries remained vulnerable and faced high risks of mortality from smallpox. It was within the poorest communities that smallpox was spread.
PART 9.3
There are medicines that could save the lives of the 500,000 children who die from malaria each year. Most of these children live in the low-income countries of Sub-Saharan Africa. Novartis manufactures the drug, artemisinin-based combination therapy, that is the standard of care for the treatment of P. falciparum malaria, the most deadly form of the disease. Although the global health community has for a long time been skeptical and wary of the private sector where profit was the driving force, Novartis happened to have a CEO who came from the field of global health and was inspired by the vision of global health equity. But neither these malaria-endemic countries nor WHO could afford to purchase commercially the amounts of this drug needed to treat the children who were at risk.