PART 8.1
In 1973 India had thousands of cases of smallpox. For a while they were reporting one thousand new cases every day. Leaders of the eradication effort wanted to solicit help from WHO and bring in physicians, epidemiologists and health worker volunteers from other countries to supplement the Indian teams. But the Minister of Health for India felt that India had plenty of health workers and volunteers to do the job and said that people from other countries were not needed. The Minister's support for the smallpox effort was essential, so the team had to convince him to support bringing in workers from other countries without being critical of the great resources India already had.
PART 8.2
In Senegal, young girls usually had to go through a painful process deeply embedded in the culture of their society that served no purpose, and had been going on generation after generation. Girls and women were advocating for an end to this practice of female genital cutting. But their pleas were not enough to convince men throughout the country to stop this traditional cultural practice.
PART 8.3
In February 2016, the World Health Organization declared the Zika virus outbreak a Public Health Emergency of International Concern. The Latin America and Caribbean (LAC) region was the most affected with more than 700,000 cases reported. In response to the outbreak, the U.S. Government allocated a portion of the funds remaining from the previous Ebola outbreak response to the LAC region. But money was not enough. The region lacked the public health and laboratory infrastructure for disease surveillance, contact tracing, and diagnostics, and needed to quickly build a workforce to respond and prevent future outbreaks.
PART 9.1
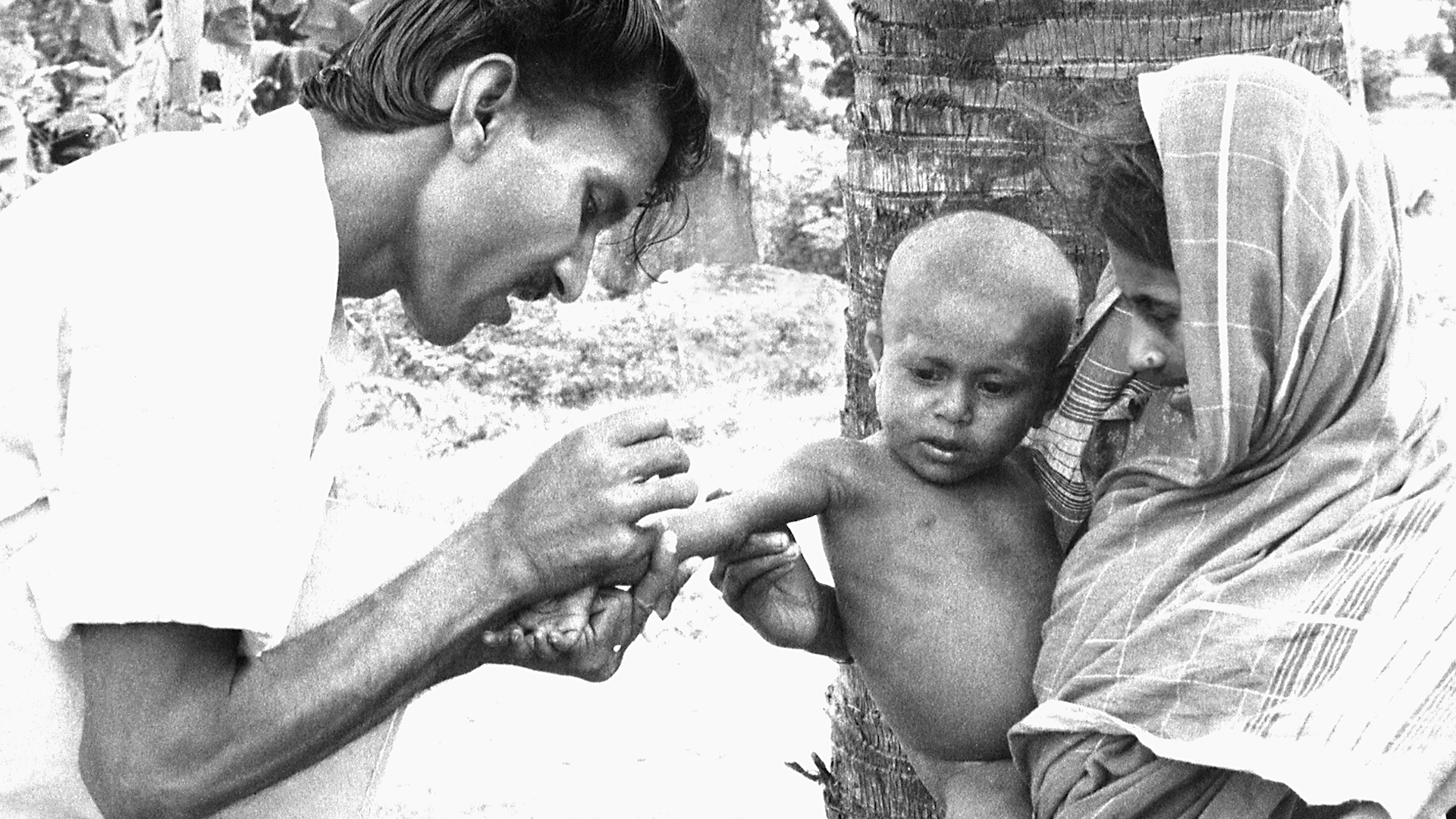
An effective vaccine for preventing smallpox had been discovered and tested by 1796. And by the 1970’s widespread vaccination resulted in most people in rich countries being vaccinated and almost completely protected. Smallpox was actually eliminated from developed countries in the 1970s. But the burden of smallpox was inequitably distributed. People in some poor countries remained vulnerable and faced high risks of mortality from smallpox. It was within the poorest communities that smallpox was spread.
PART 9.2
Partners in Health (PIH) is a non-profit global health organization established by Paul Farmer, Jim Kim, and three colleagues to bring health care to the poorest people in low-income countries. PIH believed that these people deserve healthcare that was as good as the healthcare that rich people in the most advanced countries received. They found that poor people living in a shanty town outside of Lima, Peru had very high rates of multidrug-resistant tuberculosis (MDRTB), a disease that was notoriously hard to treat.
PART 9.3
There are medicines that could save the lives of the 500,000 children who die from malaria each year. Most of these children live in the low-income countries of Sub-Saharan Africa. Novartis manufactures the drug, artemisinin-based combination therapy, that is the standard of care for the treatment of P. falciparum malaria, the most deadly form of the disease. Although the global health community has for a long time been skeptical and wary of the private sector where profit was the driving force, Novartis happened to have a CEO who came from the field of global health and was inspired by the vision of global health equity. But neither these malaria-endemic countries nor WHO could afford to purchase commercially the amounts of this drug needed to treat the children who were at risk.